Article by Megan Dunphy.
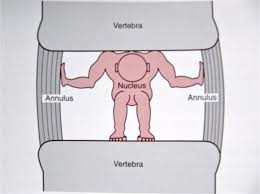
The vertebral column acts as the central flexible rod of the trunk. Each intervertebral disc, set between adjacent vertebrae, functions to both transmit load and to act as joints. The disc acts to separate the vertebral bodies allowing them to move relative to each other and thereby promoting motion at each interbody joint. Additionally, a disc must sustain the load of the body above it and the action of any surrounding muscles. In order to fulfill these functions, an intervertebral disc must be pliable yet strong.
The ability of the disc to perform these functions is largely related to the two major structural components of the tissue, the tough collagen outer casing and the proteoglycans gel nucleus. The structural collagen framework of the disc is strong in tension but collapses under a compressive load if unsupported. The proteoglycan gel nucleus draws in water to inflate the disc and is held in place by the collagen network. This enables the tissue to support compressive loads without the disc collapsing.
 The disc shows degenerative changes early in life, with 10% of the individuals aged 10-20 years having degenerate discs and with degeneration increasing steeply with age. The causes are unknown but there tends to be a strong genetic influence. There also appears to be a strong correlation between excessive loads placed on the discs over time and the onset of disc degeneration. Disc degeneration is thought to lead to back pain, either directly or indirectly. However, a degenerative disc may not be painful.
The disc shows degenerative changes early in life, with 10% of the individuals aged 10-20 years having degenerate discs and with degeneration increasing steeply with age. The causes are unknown but there tends to be a strong genetic influence. There also appears to be a strong correlation between excessive loads placed on the discs over time and the onset of disc degeneration. Disc degeneration is thought to lead to back pain, either directly or indirectly. However, a degenerative disc may not be painful.
One of the main compositional changes in degenerate discs is decreasing concentrations of proteoglycans in the heart of the disc, which results in the disc losing water content and disc height. Progressive deterioration results as the disc loses the ability to hold water under compressive forces, from both gravity and muscle.
As the disc dehydrates, load is transferred to the disc wall, which then thickens as it bunches down under compression. By taking load through its wall instead of a bubble of fluid at the center means the disc loses compliance. As the disc gets progressively flatter and stiffer, the load is transferred to adjacent spinal structures such as muscles, ligaments, facet capsules and bone, all of which are highly innervated. At the end-stage of this pathology, the disc is so degenerated that there is little liquid in the center to disperse pressure with load, the vertebral end plates are traumatized and break, allowing blood to penetrate into the disc, which nerves then follow. As a result, these degenerated discs have more blood vessels and innervation than ‘normal’ discs, and thus can become extremely painful.
Diagnosis
Early degenerative disc disease may not be painful until other surrounding tissue is affected. Once it is a suspected cause of pain, X-Rays will provide some information on disc height and associated changes to surrounding bony structures. Degenerative changes to the disc composition and structure can be seen on 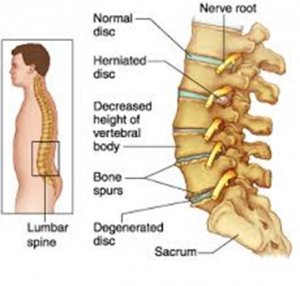 MRI.
MRI.
Treatment
In order to function well, the disc must retain a well-ordered extracellular matrix. Disc cells make and maintain this matrix, therefore any loss of cellular function will eventually lead to a loss of matrix components and disc degeneration. Therefore, treatment is focused more on prevention and maintaining well hydrated discs. A stronger core, good posture and biomechanics, result in decreased forces on the disc, aiding in preventing disc degeneration.
Initially, treatment is focused on avoiding aggravating the condition. This may be as simple as avoiding lifting heavy objects, or decreasing muscle spasm to relieve any compression in the area.
An exercise program will aid in relieving the pain of degenerative disc disease and can help prevent further degeneration. Pilates is a well-known treatment for low back pain and can assist those with degenerative disc disease by maintaining the mobility of each intervertebral segment, improve flexibility around the pelvis, strengthen deep intervertebral muscles, and improve postural awareness.
