Article by Kate Mcleod, Aug 2014
The achilles tendon is the thickest and strongest tendon in the body. It attaches the gastrocnemius and soleus muscles of the calf to the heel bone. Runners have a 30 times greater risk of developing an Achilles pain than sedentary people.
Overuse injuries are the most common type of injury presentation in the achilles region. Common symptoms associated with this diagnosis are tendon pain during or after exercise, pain that increases with increased load and a focal area of tenderness. Morning stiffness is a classic symptom of a developing achilles overuse injury.
What Causes Achilles Pain
In the past it was believed that the pathological process in this injury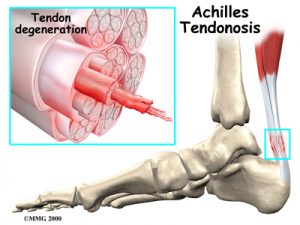 involved inflammation, with the term tendonitis applied (itis on the end of a word indicates inflammation, like tonsillitis). It is now well known that there is an absence of inflammatory cells in tendon injuries and the current understanding and management of tendon overuse injuries is based on a model of tendon breakdown, with the term tendinopathy applied.
involved inflammation, with the term tendonitis applied (itis on the end of a word indicates inflammation, like tonsillitis). It is now well known that there is an absence of inflammatory cells in tendon injuries and the current understanding and management of tendon overuse injuries is based on a model of tendon breakdown, with the term tendinopathy applied.
Although tendinopathies are the most commonly seen injury in this area, differential diagnoses such as posterior impingement of the ankle, bursitis, referred pain from the lumbar spine and rupture of the tendon need to be ruled out as part of a complete assessment. Heel pain in adolescent runners may be the result of Sever’s disease and requires a different management strategy to the injured adult runner.
Achilles tendon overuse injuries in runners usually arise from increased training volume or intensity. Increases in distance, running speed, changes in running surface and running technique can all increase the load demands on the tendon. Once the loads on the tendon exceed the the capacity of the tendon to withstand these loads, breakdown of the tendon structure occurs. When the breakdown of the tendon occurs at a rate faster than the body is able to repair, pain and injury results
Factors that predispose runners to achilles injuries include abnormal foot biomechanics, poor lower limb muscle balance, calf weakness, genetic predisposition, menopause, diabetes, ankle stiffness and calf tightness. Certain classes of antibiotics have been shown to increase the risk of an acute onset of achilles tendinopathy. Runners with a diagnosis of a sero-negative arthritis have a higher incidence of bilateral achilles problems.
Management of achilles pain should be targeted to the phase of tendon degeneration. Imaging can help grade a tendon injury, but most rehabilitation programs can be designed around the clinical signs and symptoms.
1. The initial phase of management should always be based around activity modification and reducing the load on the effected tissue to allow the body to begin the repair process. Taping, massage, stretch to the muscles and joints as well as the use of heel lifts or orthotic devices can be used effectively to offload the injured area.
2. Phase two involves a program of controlled loading to the tendon in an attempt to stimulate the body to strengthen the damaged tissue. Any biomechanical contributors to the injury are addressed at this point with corrective rehabilitation exercises. This is done in conjunction with the treatment from phase one.
3. Phase three involves ongoing increased loading to the tendon as well as a progressive increase in general exercise, with an eventual return to sport and full activity, as soon as the tendon is strong enough.
Your physiotherapist can provide you with a program individualised to address the predisposing factors and target the phase of tissue pathology. Essentially achilles injuries are an over-use and over-load injury. The cornerstone of an effective rehabilitation program is the modification and management of tendon load.


